
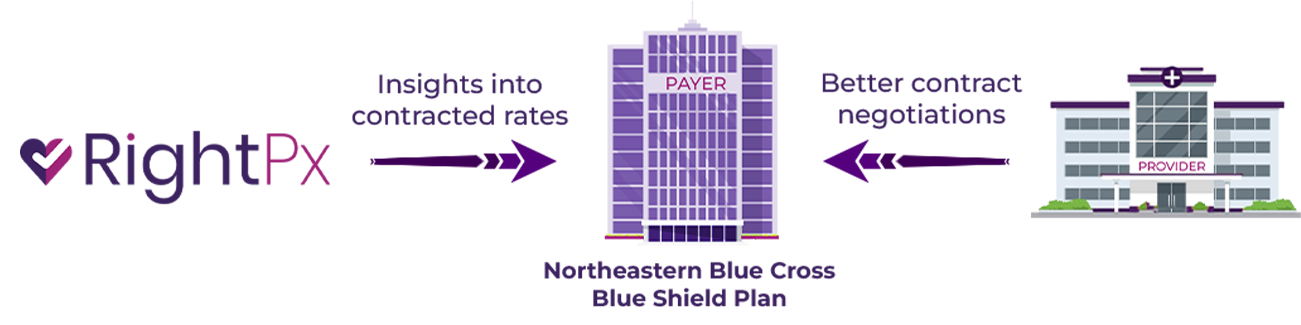
supports a Northeast Blue Cross Blue Shield Plan
Contract Negotiations
Client
A Northeastern Blue Cross Blue Shield Plan.
Challenge
Payer-provider contracts are vital for ensuring timely and appropriate reimbursement for healthcare services. To remain competitive, payers need to compensate based on market benchmarks. However, before CMS’s Price Transparency rule, competitive rate information was largely unavailable, leaving contract negotiations to proceed with minimal data. While the CMS Transparency rule has provided access to competitive data, the real challenge lies in processing, analyzing, and delivering market-specific insights.

Key Takeaways
Insights, not Data
With unlimited access to data of 100s of payers, millions of providers and billions of contracted rates, RightPx delivered curated insights specific to the counties of interest for the payer. These insights empowered the payer to make informed decisions about market entry, contract negotiations, and estimating the impact of rate changes.

Simplicity of Use
RightPx simplified the user experience by eliminating the need to navigate massive databases. With just a click, users could effortlessly compare their rates with those of other payers. Seamless data exchange ensured smooth integration with their internal databases.

Prioritizing Provider Partnerships
One of our initial goals was to utilize the rate information to foster collaboration between provider and payer, especially during contract negotiations and the past 18 months demonstrate that the goal is being realized. Enhanced efficiency coupled with improved data accuracy led to narrower rate variations across payers and a lower cost burden on members.

What is RightPx?

RightPx has the largest database of healthcare prices that can be drilled down to provide insights by payers within a region, facility, physician group, and specialty. It understands payers' behavior and payment trends by code to make informed decisions. This helps payers establish benchmarks and analyze performance relative to the competition to formulate data-driven decisions on fee schedules and new market penetration strategies. This fosters market transparency and reduces the financial burden on their members.